Fasting blood sugar levels help predict or understand how your body responds to insulin after you eat.
One of the most common health concerns related to being overweight or obese is insulin resistance. If your body cannot appropriately regulate insulin when you eat, it can have a wide variety of consequences, including weight gain and weight loss resistance, but also heart disease, chronic inflammation, and much more.
Blood sugar will normally peak about an hour after you’ve eaten a meal, after your insulin production has been called into action and is circulating in your blood, and will slowly return to normal within another hour or two. If your blood sugar spikes dramatically and doesn’t return to normal, you may have a problem with insulin resistance.
What is Insulin Resistance
Our bodies use glucose for fuel but depending on what and how much we eat in a single meal, not all of it will be immediately converted into energy. Some of it will get stored for use in the future. Insulin is the hormone responsible for deciding how much energy needs to be converted immediately, and how much glucose should be stored either as glycogen in your liver or muscles or inside your fat cells.
Insulin sensitivity means that our cells respond quickly and efficiently to insulin’s instructions. This is ideal. Many factors help keep our cells insulin sensitive, such as:
- Exercise and physical activity
- Well managed stress levels
- A healthy gut microbiota
On the other hand, low levels of physical movement, high levels of stress, and an unbalanced, unhealthy gut and impair insulin function. What’s more, poor eating habits have been very closely linked to insulin resistance.
There is only so much room in any cell for energy. When a cell is full, it will start to ignore insulin’s command to take more energy. If this happens now and then, it won’t be too much of a problem. Your pancreas will produce more insulin, it will work a little bit harder and eventually, all the glucose in your bloodstream will either be shoved into a cell as energy or as fat.
If you’re constantly consuming too much glucose, your cells will begin to pathologically ignore insulin, resulting in insulin resistance. Your pancreas will pump out more and more insulin to take care of the overflow of glucose, and in time, it will wear out as well.
If your pancreas exhausts its capability to produce enough insulin and your cells won’t take in any more glucose, your blood sugar will stay elevated.
Fasting Normal Blood Sugar
To determine your normal blood sugar levels, you can take a simple blood sugar test. There are many kits available for home use.
Doctors will normally recommend testing your blood sugar when you first wake up because this is a naturally fasted state, assuming you’ve slept 8 hours and haven’t been eating in your sleep.
You can also test your blood sugar either before you eat or at least 2 hours after you’ve eaten.
Morning Blood Sugar
To help you wake up in the morning, your body will produce a variety of hormones to trigger a stress response significant enough to alert all your senses and shake off your slumber. Cortisol, epinephrine, and norepinephrine all spike in the morning to get you out of bed.
These hormones will also release glucose into your bloodstream, so it is normal and natural to have a higher blood sugar level when you first wake up.
Fasted tests show you how well your body handles a prolonged state of glucose restriction. To monitor how it responds to food, you would have to test your blood multiple times throughout the day.
Random Blood Sugar
A random blood sugar test is any testing that is done without first being fasted. If you or your doctor is concerned about risk factors for diabetes, they may also suggest glucose tolerance tests, which will typically analyze your blood sugar levels on an hourly basis to record fluctuations.
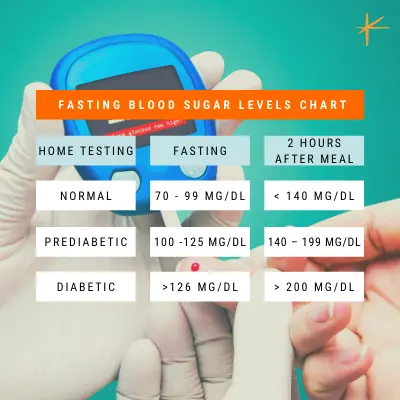
Fasting Blood Sugar Levels Chart
Every human being is unique and there is no exact number that promises perfect health when it comes to your blood sugar levels. That being said, there are ranges of normal depending on when you’ve consumed your last meal.
| Home Testing | Normal | Prediabetic | Diabetic |
| Fasting blood sugar level | 70 – 99 mg/dl | 100-125 mg/dl | > 126 mg/dl |
| Blood sugar 2 hours after a meal | < 140 mg/dl | 140 – 199 mg/dl | > 200 mg/dl |
Ketosis and Blood Sugar
Many people who follow a ketogenic diet for an extended period find that they are also insulin resistant but without any of the side effects caused by standard pathological insulin resistance, such as diabetes.
The reason for this is simple: following a keto diet adapts your body to using fat as fuel. It’s no longer accustomed to using glucose for energy and it is more likely to turn it down. Despite this resistance to carbohydrates, a fat-adapted body will continue to produce glucose through the normal process of glycolysis that our liver is in charge of, whether or not we actually consume carbs.
Certain cells inside your body require glucose to function. For this reason, our liver is perfectly equipped to convert fat and protein into glucose if we’re not eating carbs. Because the vast majority of your cells are no longer interested in consuming glucose as fuel, you may find that your blood sugar levels increase when you’re on a ketogenic diet.
It should, however, remain stable as your liver will only produce as much as is necessary. It just takes a while for the circulating glucose to reach the intended cells, hence the spike in blood sugar.
If you’re following a strict ketogenic diet, you shouldn’t worry that an elevated blood sugar level means you’re no longer in ketosis, as that’s not necessarily the case. It also doesn’t necessarily signify unhealthy insulin resistance. If, however, you start to notice other symptoms of poorly regulated blood sugar, you may want to consult with your doctor.



